Long, boring article. Until you get to the speculation that Clade I (Clade One) is mutating.
Mpox: Is The World Failing The Next Pandemic Preparedness Litmus Test?
healthpolicy-watch.news
At a time when the world is negotiating the best way forward for sustained preparedness to address pandemics, it is still exhibiting collective failure to learn from past outbreaks and a glaring gap in global health security. Mpox is one case in point – and a test case for global intent on pandemic preparedness.
In a remote village in Niger Delta Region of Nigeria, a 55-year-old man’s life was forever changed by mpox. For weeks, he suffered alone, his body and face ravaged by extensive lesions.
Shunned by local health clinics and stigmatized by his community, he endured not just the physical agony of mpox but also its profound psychological toll. By the time he reached a hospital willing to treat him, it was too late to save his vision, permanently impaired by keratitis.
In the Democratic Republic of the Congo (DRC), a mother in the Mongala province faced the agony of watching her three children suffer from mpox. The eldest child, aged seven, was the first to contract the disease. As all the children shared clothes, the younger siblings, aged four and five, fell ill too, weaving a tapestry of shared suffering.
Human cost of inaction
These heart-wrenching stories are a stark reminder of the human cost of inaction. Far from being isolated incidents, they painfully illustrate the dire consequences of global neglect in addressing mpox, particularly in Africa.
For over 50 years, this African disease has been neglected by the international community with limited or no investments in surveillance.
Despite the growing threat posed by the disease, almost no mpox vaccines and few therapeutics have reached Nigeria, DRC or other West African countries at the epicenter of the epidemic.
Moreover, critical funding for research and the development of more effective, affordable and accessible diagnostic tools, vaccines, and treatments remains woefully insufficient.
Caused by the monkeypox virus (MPXV), mpox has been endemic in most parts of central and western Africa since the 1970s, after first being discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research.
Until very recently, the more pathogenic clade I strain of the MPXV was restricted to a few Central African countries, particularly the DRC. Infants, children and young adults, mostly in rural settings and in close contact with the animal reservoir, experienced stigma, and excruciating pain due to mpox skin lesions and frequently severe disease that led to deaths.
The clade II strain, which is common in West Africa, causes less severe disease but also negatively impacts on the health and socioeconomic livelihoods of affected patients and their families.
In Africa, the disease was largely spread from animal-human spillover events, with only a few, limited cases of human-to-human transmission within households, before transmission would ‘burn out’ locally.
Unfortunately, due to poverty, weak health systems and other resource-constraints, countries, communities and families facing the challenge of mpox were unable to adequately respond and contain the disease. But the virus continued to evolve and mutate so as to be more effective in transmission to humans, including sexual transmission.
More dangerous Clade 1 infections spreading rapidly
Men queuing for the mpox vaccine in Chicago in the US. Many African countries have yet to receive mpox vaccines despite the disease being endemic in parts of central and west Africa.
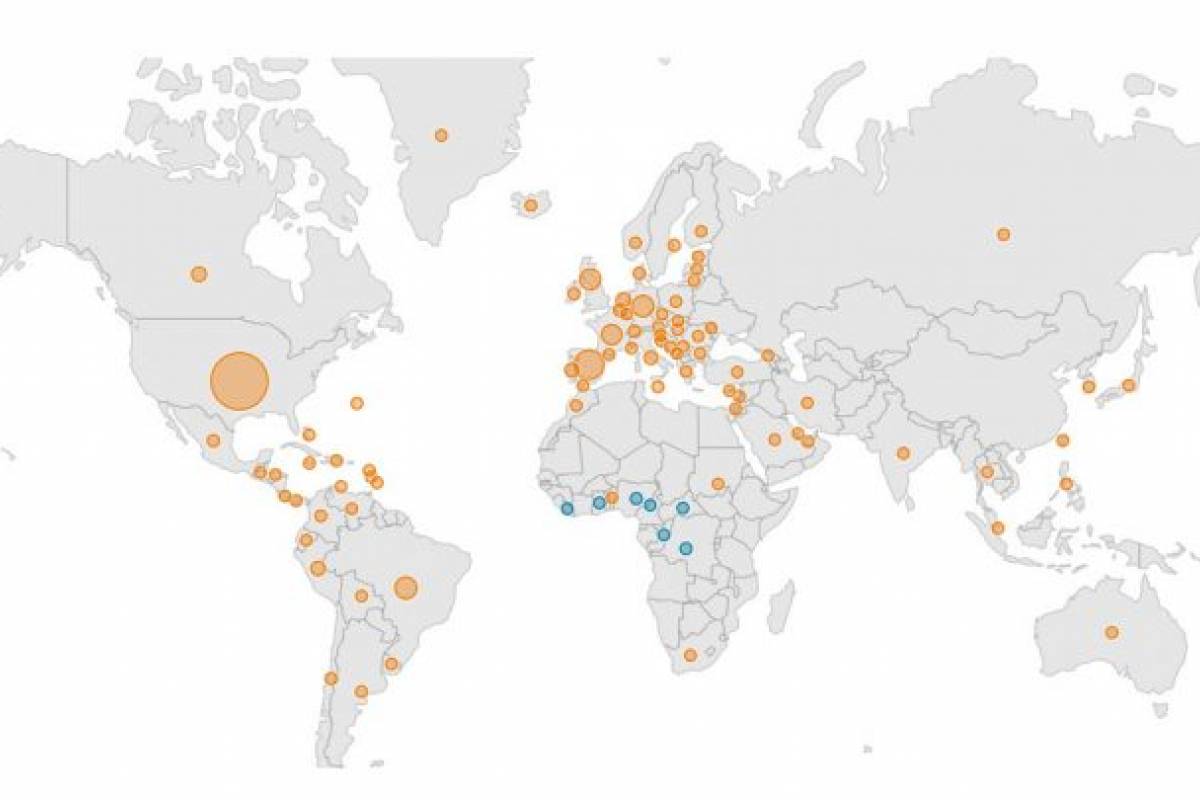
In July 2022, the World Health Organization (WHO) declared mpox a public health emergency of international concern (PHEIC) on account of the global spread of the disease to over 100 countries in all continents of the world. For the first time in history, many countries outside Africa were reporting community transmission of mpox without any travel link to previously endemic African countries.
Whereas prior outbreaks of mpox in Africa were largely zoonotic related, in 2022, mpox was unusually spreading mostly among gay, bisexual and men who have sex with men (GBMSM) by sexual contact.
The declaration of mpox as a PHEIC was intended to foster immediate and coordinated international action to contain the virus and prevent its further spread. The WHO external situation report of the 2022 multi-country outbreak has continually emphasized the significant knowledge gaps regarding route of transmission and risk factors for mpox among affected African countries.
Although mpox now seems to have been contained in most high-income countries, little has changed in West and Central Africa where the disease is endemic. The story of neglect remains largely the same.
The DRC, meanwhile, remains in the throes of its largest outbreak ever. Since January 2023, over 12,000 suspected cases have been reported in the DRC, only 9% of which were definitively laboratory tested due to resource-constraints.
In November 2023, the WHO announced the detection of clusters of mpox cases linked to sexual contact among GBMSM in the DRC, the first reports of sexual transmission of the clade I strain in history.
This unprecedented observation should be a wake-up call to re-examine investments and commitments to address the challenge of mpox in previously endemic countries, to avert another re-emergence of a global health emergency due to mpox.
The first few months of 2024 reflect an alarming surge in suspect cases and fatalities due to mpox, surpassing figures from the previous two years.
WHO responses
The WHO has developed a standing recommendation and a medium- to long-term
mpox strategic response plan. To inform development and deployment of mpox-related medical countermeasures such as therapeutics and vaccines, the WHO published
Target Product Profiles and developed a core protocol for the conduct of therapeutic clinical trials related to mpox.
Affected countries, mostly high-income countries in Europe and America, have
intensified risk communication and social mobilization, heightened surveillance and deployed existing smallpox-related vaccines and therapeutics (thought to be cross-protective against mpox) for use by the most at-risk social groups under an emergency use authorization.
These include MVA-BN, produced by the Belgium-based Bavarian Nordic and LC16 KMB, produced by Japanese firm KM Biologics.
As clinical efficacy trials on mpox vaccines and therapeutics were lacking, many collaborative efforts were initiated or strengthened, to facilitate the conduct of mpox clinical trials. These coordinated international responses led to a sustained global decline in the number of new cases of mpox and the outbreak was effectively contained in most countries outside Africa by December 2022. In May 2023, the WHO declared an end to the mpox global emergency.
While declaring the end to the mpox emergency, the Mpox Emergency Committee indicated that “the gains in control of the multi-country outbreak of mpox have been achieved largely in the absence of outside funding support and that longer-term control and elimination are unlikely unless such support is provided”.
‘Not one dollar’ to support mpox in endemic countries
And yet, as Dr Mike Ryan, Executive Director of the WHO Health Emergencies Programme, pointed out: “[mpox] is a neglected disease […]. In fact, WHO had to fund all of this international response purely on the basis of a contingency fund for emergencies. Not one dollar was received from donors to support this response and support countries.”
That means no donor funds have been available to strengthen mpox diagnosis, treatment, vaccination and control in the endemic countries like DRC, Nigeria and other neighboring countries in West Africa. Regardless of the risks posed to people in the region – or globally.
Moreover, neither of the existing vaccines, both only available in limited supplies, are ideal for low- and middle income settings. The MVA-BN requires two jabs while the LC16 KMB is administered intradermally, a procedure unfamiliar to many rank-and-file health workers in low and middle-income countries (LMICs). There is a need to fund research for adapted, affordable and available medical countermeasures.
Today only tecovirimat, an oral treatment developed by SIGA, has received approval for use, based on animal data, in the European Union (EU) and US.
When mpox cases rose, it was decided that a robust controlled clinical trial, confirming tecovirimat’s efficacy and safety in patients with mpox would be needed.
Tecovirimat has to be administered twice daily after a solid food meal, and it is being investigated in the DRC in supervised, hospitalized patients. No data have yet been generated for any other African country where Clade II occurs, nor in an outpatient setting. No other treatment has yet been investigated in patients. Tecovirimat is not approved in any African country and not yet available, even for compassionate use in Africa in clinical routine care.
Five clinical trials
Globally, there are currently only five randomized trials being conducted or planned on mpox treatments:
UNITY (Switzerland, Brazil, Argentina),
EPOXI (Europe),
STOMP (USA, International), PALM007 (DRC) and MOSA (Benin, Cameroon, Central African Republic, Congo Republic, DRC, Ghana, Liberia and Nigeria).
All the trials are testing tecovirimat as monotherapy. STOMP and PALM007 are funded through NIH/NIAID. MOSA is a platform adaptive trial in Africa that could test other treatment arms, which is supported by PANdemic preparedness plaTform for Health and Emerging infectious Response (PANTHER).
Horizon Europe is funding mainly the EPOXI trial in Europe, although it is also providing some support to UNITY.
However, there is still a large funding gap to cover for the completion of those trials, especially in Africa. Furthermore, whereas various north south collaborations between African scientists and other researchers from across the globe are ongoing, there are still glaring gaps in investments in mpox surveillance, as well as available diagnostics and treatments in affected countries.
In Africa, children worst affected
While in the Clade II global health emergency, most of the victims were men, in Africa, the Clade I victims are now mostly children under the age of 16.
The number of skin lesions that each person with Clade I experiences is much higher – up to several hundred in comparison with tens in Clade II. Bacterial infections and underlying malnutrition can increase morbidity and the case fatality ratio is definitely higher in Africa than in high income countries. Those features are contextual and must be considered during drug development as they may significantly affect treatments’ strategies and overall efficacy.
At the same time,
if mutations in Clade I mpox in the DRC are changing the pattern of infection and transmission, then new treatments are all the more critical to not only end the local outbreak but to prevent it from spreading more widely via sexual contact and other means.
Test of humanity
The tardiness of action on mpox demands an immediate and concerted effort from the international community. By prioritizing research and vaccine development, enhancing international collaboration, and addressing stigmatization, we can strengthen our global preparedness for emerging health threats. As recently stated by Africa CDC, “vulnerable populations worldwide must have access to life-saving interventions”.
We stand at a crossroads between repeating past oversights and forging a new path of true equity and foresight. We cannot afford to repeat the mistakes we made over Ebola when funding was only made available when high-income countries were at risk.
It is time to harness the spirit of international collaboration. Building on positive initiatives like the UNITY trial, nations must come together to address the unique challenges posed by mpox and respond to the specific needs of African patients.
Mpox isn’t just a test of our global intent on preparedness – it’s a test of our humanity. In honoring the memory of the young victims, like an eight-day-old baby girl in DRC, we must pledge to do better, act faster, and create a global health infrastructure that is as inclusive as it is effective.
Prof Jean-Jacques Muyembe Tamfum is the Director General of the DRC’s National Institute of Biomedical Research (INRB) in Kinshasa, Professor of Microbiology at the University of Kinshasa Medical and the inaugural president of the Congolese Academy of Science. He is co-discoverer of the Ebola virus in 1976 and co-inventor of the monoclonal antibody “ mAb114”, approved by FDA as an Ebola treatment, Ebanga, in December 2020. The INRB is conducting the PALM007 study on Tecovorimat in mpox patients.
Prof Dimie Ogoina is a Professor of Medicine and Infectious at the Niger Delta University Teaching Hospital in Nigeria. Ogoina’s team were the first to describe sexual transmission of mpox in Nigeria in 2017. He was a member of the World Health Organization IHR Emergency Committee on the multi-country outbreak of mpox.
Prof Francine Ntoumi is head of the Congolese Foundation for Medical Research, which she founded 15 years ago. She has over 20 years of experience in basic and clinical research in infectious diseases particularly malaria, HIV and tuberculosis, in endemic countries and Europe.
Dr Nathalie Strub Wourgaft has been Delegate General for the PANdemic preparedness plaTform for Health and Emerging infectious Response (PANTHER) since its creation in 2022. Prior to that, she was Director of NTDs and later for COVID and pandemic preparedness at the Drugs for Neglected Diseases Initiative (DNDi) from 2009 to 2022.
Prof Samba Sow is Director of CVD-Mali. A medical doctor and epidemiologist, Sow was Minister of Health and Public Hygiene for Mali between April 2017 and May 2019 and instituted a series of health sector reforms to provide free antenatal and maternal healthcare as well as free care for children under five years old. In 2020, he was appointed WHO Special Envoy for COVID-19 in West Africa.
Image Credits:
TRT World Now/Twitter .
Combat the infodemic in health information and support health policy reporting from the global South. Our growing network of journalists in Africa, Asia, Geneva and New York connect the dots between regional realities and the big global debates, with evidence-based, open access news and analysis. To make a personal or organisational contribution click here on PayPal.
At a time when the world is negotiating the best way forward for sustained preparedness to address pandemics, it is still exhibiting collective failure to

healthpolicy-watch.news

www.newspressnow.com