Radagast just did a piece on bird flu today, I'll add it to go with that tweet. Keep in mind though he is a very strong proponent of vegetarianism which is evident in this piece.
(fair use applies)
What nobody wants to hear about bird flu
Radagast
November 3, 2024
Look, this is my blog, so I get to decide what I want to write about. I don’t have a bunch of fat American MAGA boomers sending me 5 dollars a month in exchange for telling them that Joe Biden’s climate change hysteria is going to make our meat and eggs expensive.
I look at this website a bit like my legacy. I will die one day and then I’ll be able to take comfort in the fact that I sought to tell people the truth, instead of the popular lie that makes you money. I don’t have to administer you addictive brain-opioids, that lull you to sleep. I get to tell you what you don’t want to hear. I get to tell you, the truth. People don’t lie to you to deceive you. They lie to you because you prefer being lied to.
But this is the truth and you’re not going to like it. The bird flu, is not “flu”. Yes, it’s technically an influenza virus, in the same sense as a bat is technically a mammal. But when you think of a mammal, you think of an animal that lives on land, not an animal that flies in the sky.
How many influenza viruses can you think of, that kill an animal by destroying the blood vessels in its brain?
That’s what the “bird flu” does to cats. It turns the brain to mush.
Why? Because it has a polybasic cleavage site. What does that mean in simple English? A protein is made of amino acids. There are 22 of those found in the genetic code of life. Three of those, Arginine, Lysine and Histidine are
basic amino acids, the opposite of acidic.
When you put a whole bunch of those basic amino acids close together in a protein, you get a polybasic site. This allows enzymes our cells produce to attach there. Those enzymes can then cut up the protein at that particular site.
The effect this has, is that when a protein of a virus develops such a polybasic site in the exact right spot, it can start to infect different cell types, cell types that produce these particular enzymes, that would normally not be available for such a virus to infect. One of those enzymes is furin, but there are others too. That’s why you hear this term “polybasic furin cleavage site” thrown around a lot, about SARS-COV-2.
But the influenza virus, that we know for causing “the flu”, normally has no polybasic cleavage site. It only has been found to develop the polybasic cleavage site,
under two conditions:
-Cell cultures in a lab.
-Massive factory farms full of birds
And we know why this is. With at least five of these basic amino acids in a row, you call the cleavage site “polybasic”. When you see three or four of these basic amino acids in a row, you call the cleavage site “multibasic”. Normal influenza, the type that infects us humans and other animals, has just one basic amino acid, that only allows enzymes found in our lungs to cleave it. We call this “monobasic”.
And the problem is as following: To get to the polybasic cleavage site variety as a virus, you first have to evolve the multibasic variety, out of the monobasic variety. But the multibasic variety, is just not very good at functioning as a virus. It’s bad at competing in the wild.
On the other hand, when such a virus emerges in a factory farm, where it faces no competition from other viruses, no pre-existing immunity against influenza and birds with poor health, it can easily spread there, mutate to add more basic amino acids and evolve into the polybasic cleavage site variety. And unlike the intermediary step, the multibasic variety, the polybasic variety
does manage to survive in the wild, so now wild birds can start spreading it from one chicken broiler to another.
I’ll quote the study for you:
Low pathogenicity avian influenza viruses (LPAIVs) are generally asymptomatic in their natural avian hosts. LPAIVs can evolve into highly pathogenic forms, which can affect avian and human populations with devastating consequences. The switch to highly pathogenic avian influenza virus (HPAIV) from LPAIV precursors requires the acquisition of multiple basic amino acids in the haemagglutinin cleavage site (HACS) motif. Through reverse genetics of an H5N1 HPAIV, and experimental infection of chickens, we determined that viruses containing five or more basic amino acids in the HACS motif were preferentially selected over those with three to four basic amino acids, leading to rapid replacement with virus types containing extended HACS motifs. Conversely, viruses harbouring low pathogenicity motifs containing two basic amino acids did not readily evolve to extended forms, suggesting that a single insertion of a basic amino acid into the cleavage site motif of low-pathogenic viruses may lead to escalating selection for extended motifs. Our results may explain why mid-length forms are rarely detected in nature. The stability of the short motif suggests that pathogenicity switching may require specific conditions of intense selection pressure (such as with high host density) to boost selection of the initial mid-length HACS forms.
That last sentence I made bold, because this is the important thing to understand: These viruses are NOT natural! They’re a product of humans putting birds in these conditions:
When you put the birds in HELL, you give birth to a virus from HELL.
This thing was born in the 90’s in China. They tried vaccinating against it, but it didn’t work, it just accelerated its evolution and encouraged it to spill over into other animals.
The important thing to understand is as following: It’s the polybasic cleavage site,
that allows influenza viruses to infect endothelial cells, in humans as well as in birds. Remove the polybasic cleavage site and it becomes like normal influenza, in that it can’t replicate in the endothelial cells anymore. I quote:
To test the permissiveness of pulmonary endothelial cells to virus infection, we compared the replication of selected seasonal, pandemic (2009 H1N1 and 1918), and potentially pandemic (H5N1) influenza virus strains. We observed that these cells support productive replication only of HPAI H5N1 viruses, which preferentially enter through and are released from the apical surface of polarized human endothelial monolayers. Furthermore, A/Thailand/16/2004 and A/Vietnam/1203/2004 (VN/1203) H5N1 viruses, which exhibit heightened virulence in mammalian models, replicated to higher titers than less virulent H5N1 strains. VN/1203 infection caused a significant decrease in endothelial cell proliferation compared to other subtype viruses. VN/1203 virus was also found to be a potent inducer of cytokines and adhesion molecules known to regulate inflammation during acute lung injury. Deletion of the H5 hemagglutinin (HA) multibasic cleavage site did not affect virus infectivity but resulted in decreased virus replication in endothelial cells.
The endothelial cells, are the cells that line all your blood vessels, including in your brain.
Different cell types, will have different machinery operating inside of them. When the virus develops the polybasic cleavage site that allows it to switch to the endothelial cells, that means it has to figure out how to make optimal use of those cells, rather than the cells in the lungs it would normally rely on.
So what happens next is that
the internal genes start to change too, to enable efficient use of the new cell types it can infect. The polybasic cleavage site makes the virus deadlier, but
it’s not enough on its own to get the results we now see in the chickens, where 90% of them die within 48 hours of infection. All sorts of other changes start to happen, once the virus has the polybasic cleavage site.
This is why it’s insanity, to expect that once the bird flu becomes a virus that jumps between humans, it will eventually evolve to become like the normal flu we’re used to.
Do you expect whales to crawl back on land again at some point? Do you expect bats to lose their wings one day and live like mice? When such a sudden dramatic shift happens in the cell types this virus uses to survive in, it becomes forced to adapt to those conditions. It can’t just lose the polybasic cleavage site and go back to being a normal influenza virus, because then without the polybasic cleavage site, it still has those other mutations. So then it’s just a poor influenza virus, unable to compete with other influenza viruses.
Some of those other mutations involve
big deletions of twenty amino acids in a row. You don’t just reverse a mutation like that, that’s incredibly hard for natural selection to do.
Once this virus goes human-to-human, people imagine it will be like the 1918 influenza pandemic. First a whole bunch of people die, but then it mutates and starts behaving like a normal flu virus. That’s not going to happen.
To start with, we never see it grow milder when it’s given to animals. In such animal passage studies, it grows deadlier with every jump it makes. That’s what you’re seeing with the cows right now too, it was pretty mild in Texas when we first discovered it in cows, but now in California it’s killing huge numbers of them.
But second, it’s always going to behave like a fundamentally different virus from the influenza we know.
The 1918 H1N1 virus, did
NOT have a polybasic cleavage site. The 1918 virus, can NOT infect endothelial cells. So it can’t offer you lessons for what’s going to happen now. The polybasic cleavage site, is a consequence of our factory farms. Those factory farms, are a new thing:
So we have never seen anything like this virus in our population before, because we never before created the conditions in which a virus like this can come into existence.
It’s not going to behave like any influenza viruses that we are used to.
And it’s not just going to return to behaving like a normal influenza virus after a few waves through our population.
I will readily admit, that I love a good horror story. But modern animal agriculture, is much better at creating horror stories, than I can ever hope to be.
This is the reality of what we’re dealing with.
When you hear about bird flu on the news, those people should be reminding you of these four points:
- It does not behave like a normal flu virus.
- It’s not natural, it could only come into existence in our giant chicken broilers.
- It’s not just going to turn into a normal flu again eventually.
- It damages the blood vessels in your brain.
Those are the facts. When they are not telling you those four points, then they’re just training you to say “it’s all bullshit”. You will say: “Oh the flu? I’ve had the flu before.”
I honestly really don’t care how many people it kills, it’s going to be a horror show either way. Your endothelial cells lining your blood vessels, are basically part of your immune system. Unlike most cells, they are able to produce huge amounts of Interferon alpha, a molecule basically designed by evolution to interfere in every step of a viral reproduction cycle.
That’s what we see in this virus, it causes the infected cells
to produce huge amounts of it.
So you end up with this virus in the blood vessels in your brain. They produce huge amounts of Interferon Alpha.
You can reliably induce depression in a person, by injecting them with interferon alpha, which is sometimes done to treat a viral infection. They suffer severe depression for weeks afterwards, often it recurs later on.
Even if you survive it, it’s a virus that’s going to screw with your mind, by putting your immune system in your brain on high alert, kind of similar to SARS-COV-2.
What we see in cows right now, is that it damages the immune system, they tend to succumb not to the direct effects of the virus itself, but to subsequent bacterial infections. Again, it’s not a normal flu virus. It is found to replicate much better in myeloid cells than normal influenza. What are those? Blood cells derived from bone marrow. It includes neutrophils, macrophages and other cells of your innate immune system.
They’re going to try to vaccinate against it, which will go about as well as you would expect. We have
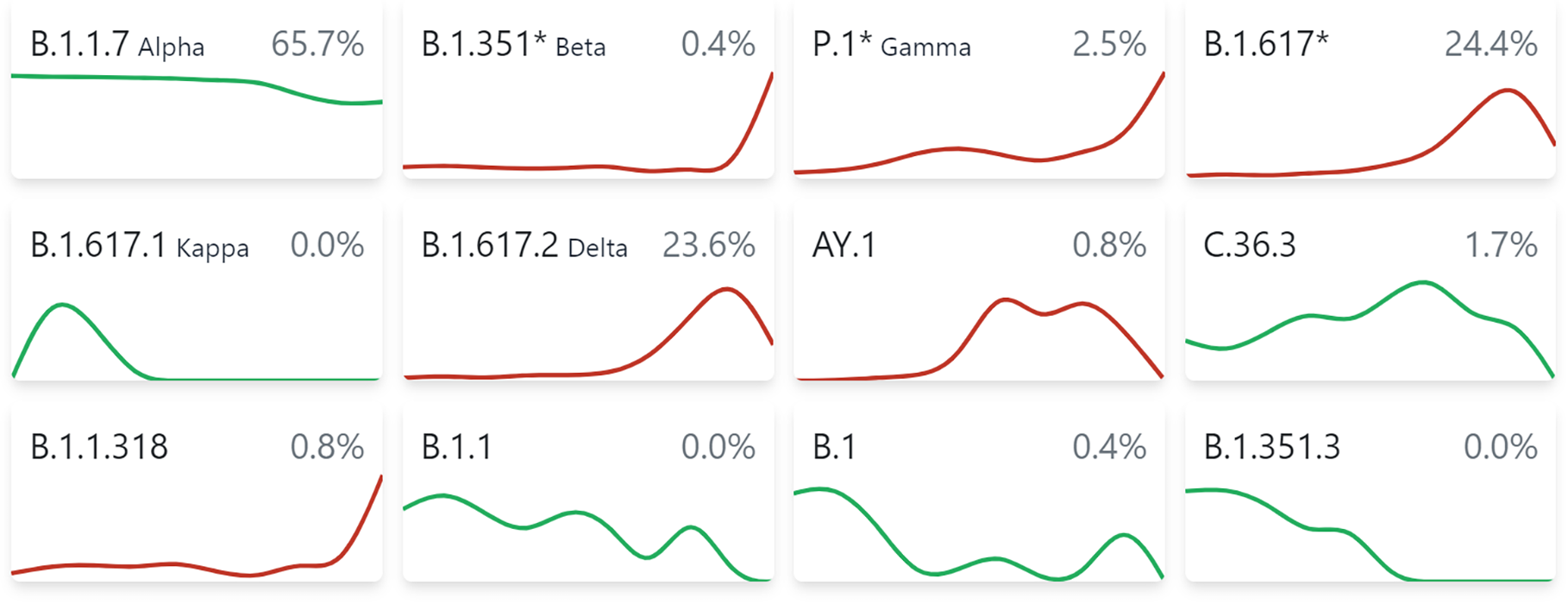
at least three separate strains now in the United States, including one jumping from chickens into humans and one jumping from cattle into humans.
The virus evolved in chickens who were being actively vaccinated against it. It’s inherently vaccine-resistant and
humans already have adaptive immunity against it from exposure to regular influenza. So the vaccines are not going to do much against it. Vaccination just selects for neurovirulence, as the antibodies normally don’t pass the blood brain-barrier.
My hope is that at least some of the population will have protection from
the natural killer cells and monocytes that migrate into the brain when you are infected by SARS-COV-2 without having been vaccinated. They don’t migrate into the brain when you’re infected while vaccinated, in which case your body just deploys antibodies that are not going to be neutralizing for influenza. The endothelial cells themselves should also have been trained by now.
It’s not looking good. But people just entirely don’t care, I’m accused of fear-mongering. The reality is: Twenty percent of your cows in California are dying from this. It
killed 96% out of 17,000 of the elephant seal pups in South America.
It’s already causing ecological disasters around the world. But people don’t want to see it, the right wingers want to think Bill Gates and Klaus Schwab invented this to force them to eat bugs. But that’s honestly not half as stupid, as the “I believe in science” types, who think we’re going to solve this by vaccinating anything that moves.
We tried that in the 90’s, when it first showed up in our poultry. It didn’t work.
It made it worse, by increasing the genetic diversity of these viruses, thereby allowing them to jump into more animal species. That’s why we are where we are now.
Sorry, but this is the story that’s going to dominate the remainder of your life. Resource depletion and climate change are big problems, but they ramp up slowly. This one, this one ramps up fast.
How do you expect to run a farm and produce milk, when half your cows die in a single month? That’s the reality some farmers in California now face.
Something like this just bankrupts farmers. And at first the government may try to prop up the farmers to keep business as usual going. But eventually you realize that it just no longer works. You can just no longer produce milk at an affordable price and your workers are bleeding from their eyeballs. That’s when entire villages in places like South Dakota, where milk is the only thing being produced, just become non-viable. Anyone who is not directly involved in producing milk there, is indirectly dependent on it.
We closed our eyes for a tragedy that happens on a constant basis:
2 min 26 sec
View: https://www.youtube.com/watch?v=HXJrk5vF4R8
So now we’ll face one of our own.
.