The peer-reviewed study published this week also found SV40 DNA contaminants in the vaccines, and the researchers also determined that the spike proteins produced by the vaccines persist in the body longer than claimed.

childrenshealthdefense.org
(fair use applies)
DNA Contamination in Pfizer COVID Vaccines Up to Four Times Legal Limits, Study Finds
The peer-reviewed study published this week also found SV40 DNA contaminants in the vaccines, and the researchers also determined that the spike proteins produced by the vaccines persist in the body longer than claimed.
by Michael Nevradakis, Ph.D.
December 4, 2024
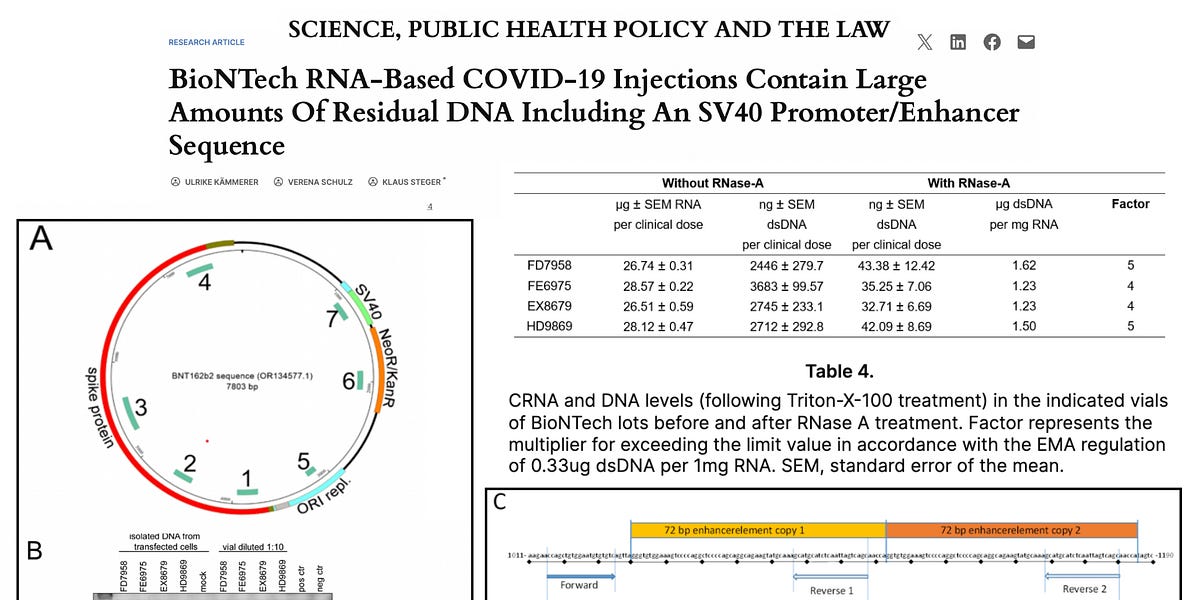
Researchers found DNA in Pfizer’s COVID-19 vaccines at levels three-to-four times higher than regulatory limits, according to a new “bombshell” study.
“This far exceeds the maximal acceptable concentration of 10 ng [nanograms] per clinical dose that has been set by international regulatory authorities,” the authors wrote.
The peer-reviewed study, published this week in the journal Science, Public Health Policy and the Law, also found simian virus 40 (SV40) DNA contaminants in the vaccines. And the researchers determined that the spike proteins produced by the vaccines persist in the body longer than claimed.
The findings led the authors to call for “an immediate halt of all RNA biologicals.”
Karl Jablonowski, Ph.D., senior research scientist at Children’s Health Defense (CHD), told The Defender that DNA contamination may contribute to the increase in autoimmune diseases among the vaccinated. “The immune system operates on very sensitive detections to initiate responses,” he said.
“DNA suddenly deposited into your bloodstream could kickstart the interferon response,” Jablonowski said. “The interferon response, when there’s nothing to find but ‘self,’ could be the springboard for autoimmune disease.”
The study also showed that the spike proteins produced after vaccination persist in the body for at least seven days following vaccination instead of the shorter period Pfizer-BioNTech previously claimed. The spike proteins are also prone to shedding.
These results “raise grave concerns” about mRNA vaccines, the study concluded.
Kevin McKernan, founder of Medicinal Genomics, is the first scientist who identified the presence of SV40 in the mRNA vaccines. He called the new study “a tour de force on the DNA contamination topic.” McKernan wrote about the study on Substack, and said in an X post that the study’s authors “knocked it out of the park.”
Immunologist and biochemist Jessica Rose, Ph.D., agreed. “This paper is the paper of the century. The paper is not only a work of art in terms of the study layout. It is very well-written and settles ongoing ‘issues’ pertaining to allegations made by regulatory bodies that the DNA contamination issue is misinformation,” Rose said.
Dr. Angus Dalgleish, professor of oncology at St George’s, University of London, told The Defender the study “diligently used techniques proving that these samples contain large amounts of DNA” and that “these samples easily enter and express in a known kidney cell line used as a standard to examine these phenomena.”
The new study follows the recent publication of a peer-reviewed paper in the Journal of American Physicians and Surgeons, identifying serious safety concerns in the mRNA COVID-19 shots. The authors of that study called “at minimum” a moratorium on the shots.
The papers join a growing list of scientists and organizations calling for a ban on COVID-19 mRNA vaccines. They include Florida’s surgeon general, the Association of American Physicians and Surgeons, Doctors for COVID Ethics, Americans for Health Freedom and the World Council for Health.
In October, Idaho’s health board voted to stop offering COVID-19 vaccines at its 30 clinics because of safety concerns. Also that month, the Slovak government issued a report proposing a ban on “dangerous” mRNA vaccines.
The new study comes amid the launch of an online library, the SARS-CoV2 Spike Protein Pathogenicity Research Collection, a database of over 250 peer-reviewed studies detailing the risks posed by spike proteins.
Dalgleish said the latest study “completely confirms” the Journal of American Physicians and Surgeons paper. “The two together should be enough legal evidence to call for the immediate ban of mRNA vaccines.”
COVID mRNA shots ‘have a dangerous mechanism of action’
In an interview with The Defender, Klaus Steger, M.D., Ph.D., professor of molecular andrology at the University of Giessen in Germany and corresponding author of the new study, analyzed the study’s findings and their significance.
The study found the presence of “residual DNA in modRNA [modified mRNA]-based Pfizer-BioNTech genetic vaccines, the concentration of which far exceeds the limits set by the international regulatory agencies. Importantly, a significant amount of this residual DNA is packaged within lipid nanoparticles,” Steger said.
According to Steger, this is significant because the lipid nanoparticles can deliver the DNA throughout the human body. He said:
“The first problem is that the existing limits set by the international regulatory agencies apply to ‘naked DNA,’ like the residual DNA in drugs produced in genetically modified bacteria, e.g., insulin or some antibiotics.
“However, DNA in the modRNA-based genetic vaccines, together with the modified mRNA, is packaged within lipid nanoparticles and thus is delivered unnoticed by our immune system into our cells.”
McKernan said the study shows that DNA is “getting into cells and not degrading.” According to Steger, “Due to the … safety risks of DNA packaged within lipid nanoparticles, the limit value for DNA must undoubtedly be zero.”
Another key finding according to Steger is the identification of two copies of an “SV40 promoter/enhancer sequence.” Steger said this SV40 sequence can “act in human cells … to encourage nuclear transport of plasmid DNA,” raising “safety concerns of unintended genomic integration of residual DNA” from the plasmid.
The presence of SV40 “increases the risk for the plasmid-DNA of being transported into the cell nucleus and probably integrated into the genome,” Steger said.
Jablonowski said SV40 penetrates the barriers of human cells, transferring foreign DNA directly into the nuclei, “violating that which ought to remain inviolable.”
Steger said the results also show “robust spike protein production by cultured cells.” The produced spike proteins “did not stay parked on the cell membrane” at the injection site, but were “packaged into exosomes.” According to Steger, “This means that the produced spike protein may be exported all over the body.”
Cardiologist Dr. Peter McCullough told The Defender the “mRNA COVID-19 vaccines have a dangerous mechanism of action. They contain the genetic code for the potentially lethal SARS-CoV-2 spike protein. Once injected into the body, there is no way to control their biodistribution, duration or quantity of spike protein produced.”
“As a result, some victims must have maldistribution, over-produce spike protein, or have susceptibilities to its cellular and tissue-damaging properties,” McCullough said.
Christof Plothe, D.O., a member of the World Council for Health steering committee, told The Defender the study showed that the presence of spike proteins lasted more than seven days, contradicting “earlier models that suggested the spike proteins would remain anchored at the injection site and dissipate within 48 hours.”
Plothe said the study also demonstrated that shedding of the spike proteins is also possible. “The research showed that the spike proteins are not merely stuck to the cell membrane — instead, they are packaged into exosomes, which are tiny vesicles that can be released from cells and potentially travel throughout the body.”
“This finding has major implications for the concept of ‘shedding,’ suggesting that if exosomes contain plasmid DNA, it could be transmissible and might even have the ability to replicate, posing additional risks,” Plothe said.
According to Steger, these mechanisms and risks are not limited to the Pfizer-BioNTech COVID-19 shots but are true of all mRNA vaccines. He said:
“The problems pointed out by our study represent general problems typical for this new type of modRNA genetic vaccine, their production process and their mode of action.
“This means that independent of the type of future plasmids applied in the production process, modRNA genetic vaccines will act in an identical way — namely, they genetically transfect our body cells and convert them into production facilities for a foreign viral antigen without any control mechanisms on unwanted negative side effects.”
Steger said this poses significant dangers for human health — including risks that could be passed on to offspring.
“This not only bears the undeniable risk of causing an autoimmune disease, but with regard to the residual plasmid DNA, raises the safety risk of DNA delivery to the cell nucleus and insertion into the genetic material — and in a worst-case scenario, even to the offspring,” Steger said.
Pfizer has previously acknowledged the presence of SV40 in its COVID-19 shots “but has downplayed any associated side effects,” Plothe said. Jablonowski noted that Pfizer and BioNTech have the resources to conduct such a study — but haven’t.
“This paper is within Pfizer-BioNTech’s capabilities,” Jablonowski said. “Yet, three researchers pieced together a highly technical effort with no external funding, showing that Pfizer-BioNTech endangered everyone injected with their product.”
“This paper explains why we have witnessed record injuries, disabilities and death after COVID-19 vaccination,” McCullough said. “There are calls from all over the world to remove these products from human use. The only way to stop further harm is to shut down the COVID-19 vaccination campaign.”
Joseph Sansone, Ph.D., author of the “Ban the Jab” resolution adopted by 10 Florida counties, told The Defender he supports the authors’ call for a moratorium. He said the study “raises serious concerns about genetic changes and the potential to predispose future generations to cancer and other diseases.”
New database of spike protein studies contributes to calls to ban mRNA shots
Steger said his paper was the target of scientific censorship. His team previously submitted the study “to two other journals, both with their main focus on vaccines.” However, both journals “returned the manuscript immediately” without reviewing it.
That led to the development of the SARS-CoV2 Spike Protein Pathogenicity Research Collection — a database of “over 250 peer-reviewed scientific studies confirming that the spike protein is highly pathogenic on its own.”
Erik Sass, a research assistant for the project, told The Defender, “This collection of research demonstrates that the SARS-CoV2 spike protein can inflict harm on the human body through a remarkably wide range of mechanisms.”
The database “also advances our understanding of the causes and possible treatments for ‘long COVID’ and vaccine injuries resulting from uncontrolled production of the spike protein throughout the body,” Sass said.
Sass said the database contains studies “published in reputable scientific journals following peer review,” but that many “formerly respected scientific publications have deviated from the high standard of intellectual integrity that made them authoritative.”
According to Sass, the project was inspired by the publication of “Toxic Shot: Facing the Dangers of the COVID ‘Vaccines’” in June — particularly its chapter on spike proteins. Sass was one of the researchers who contributed to that chapter.
“As more and more research emerged, we decided to continue adding to the collection to turn it into a standalone resource for general reference,” Sass said.
Brian Hooker, Ph.D., chief scientific officer for CHD, called the new database “a great resource for both practitioners looking for treatment options as well as scientists studying the very obvious toxicity of the COVID-19 vaccine and SARS-CoV-2 spike protein.”
“We need directly accessible information for what the future holds for addressing the myriad chronic illnesses caused by spike protein exposure,” Hooker said. For Dalgleish, the database “constitutes overwhelming evidence” that the spike protein “is highly dangerous and its use must be halted immediately.”
“Studies like ours are now being published at ever shorter intervals and occasionally find their way into the mainstream media,” Steger said. “It is only a matter of time before the house of cards of ‘safe and effective vaccinations’ will collapse.”

www.dailymail.co.uk