Heliobas Disciple
TB Fanatic

U.S. reports record single-day spike of 63,200 new cases of coronavirus
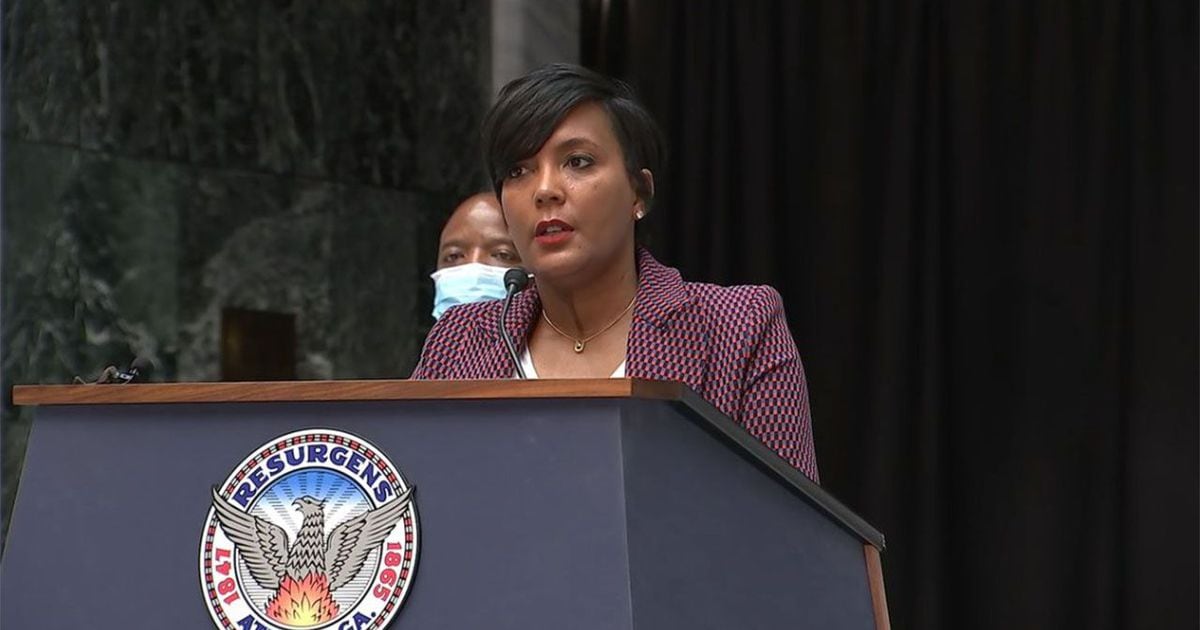
White House health advisor Dr. Anthony Fauci has urged officials in states where the outbreak is worsening to reconsider reopening plans.
U.S. reports record single-day spike of 63,200 new cases of coronavirus
Will Feuer
Published Fri, Jul 10 20208:42 AM EDTUpdated Fri, Jul 10 202010:39 AM EDT
Key Points
- It’s the second time this week the U.S. topped its record for coronavirus cases reported in a 24-hour period.
- Cases were growing, on average, by at least 5% in 36 states and the District of Columbia as of Thursday, according to a CNBC analysis of data collected by Johns Hopkins University.
- Coronavirus-related deaths are beginning to tick up in several hot spots.
The United States reported a daily record of 63,247 new cases of Covid-19 on Thursday, according to data compiled by Johns Hopkins University.
It’s the second time this week the U.S. topped its record for new infections reported in a 24-hour period as outbreaks expand across a number of states, mostly across the American South and West. California, Florida and Texas reported more than 30,400 new cases collectively on Tuesday, according to data from Hopkins, accounting for nearly half all new cases in the U.S.
The U.S. has reported about 53,699 new cases on average over the past seven days, a record high seven-day average, up nearly 17.6% compared with a week ago, according to a CNBC analysis of data collected by Johns Hopkins. The U.S. seven-day average has hit a new record every day for more than two weeks, according to CNBC’s analysis.
White House health advisor Dr. Anthony Fauci has warned that the U.S. is “not in total control” of the coronavirus pandemic and daily new cases could surpass 100,000 new infections per day if the outbreak continues at its current pace.
“What we are seeing is exponential growth. It went from an average of about 20,000 to 40,000 and 50,000. That’s doubling. If you continue doubling, two times 50 is 100,” Fauci said Wednesday on a Wall Street Journal podcast. “Any state that is having a serious problem, that state should seriously look at shutting down.”
Fauci has urged officials in states where the outbreak is worsening to reconsider their reopening plans. Instead of totally shutting down or totally reopening, Fauci told lawmakers on Thursday, states should constantly update their restrictions, tailoring them to what is currently known about the virus.
Without aggressive action, Fauci previously told lawmakers, the outbreak is “going to be very disturbing.”
“We are now having 40-plus-thousand new cases a day. I would not be surprised if we go up to 100,000 a day if this does not turn around, and so I am very concerned,” Fauci said at a June 30 hearing held by the Senate Health, Education, Labor and Pensions Committee.
Cases were growing, on average, by at least 5% in 36 states and the District of Columbia as of Thursday, according to a CNBC analysis of data collected by Hopkins. CNBC uses a seven-day trailing average to smooth out spikes in data reporting to identify where cases are rising and falling.
Coronavirus-related hospitalizations are also up, on average, by at least 5% in 25 states, according to CNBC’s analysis of data compiled by the Covid Tracking Project, an independent volunteer organization launched by journalists at The Atlantic.
Some of the rise in total cases is likely due to increased testing. Nationally, the U.S. has ramped up screening from an average of just over 174,000 diagnostic tests per day through April to more than 650,000 tests per day in July, according to the analysis of data compiled by the Covid Tracking Project. However, the percent of tests coming back positive has also risen, which epidemiologists say is a sign of a virus that is spreading more rapidly.
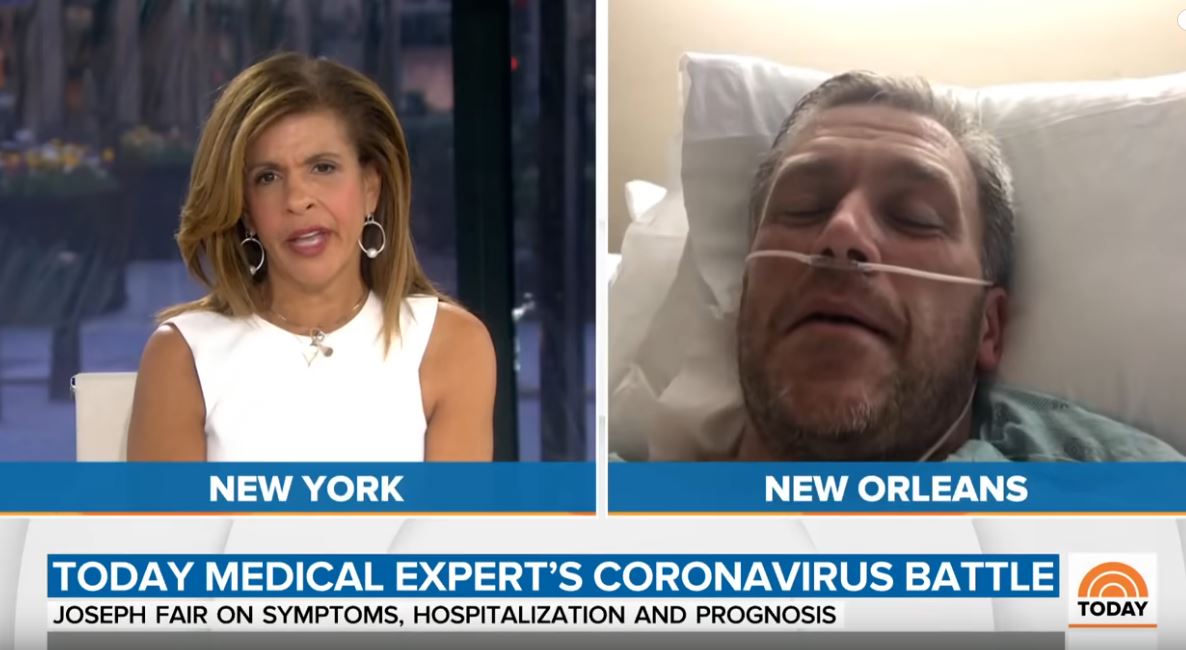
While new cases have continued to soar, deaths caused by Covid-19 have remained relatively stable and comparatively low. Fauci and other health officials have attributed this better treatment strategies and clinical care for Covid-19 patients as well as to the comparatively low average age of people infected with the virus now. The average age of a Covid-19 patient has dropped by about 15 years compared with the beginning of the outbreak, and younger people have lower fatality rates.
However, coronavirus-related deaths are beginning to tick up in several hot spots. The seven-day average of newly reported deaths caused by Covid-19 hit record highs on Thursday in six states: California, Florida, South Carolina, Tennessee, Texas and Utah.
However, Fauci has warned that Covid-19 deaths lag a few weeks behind diagnosis of new cases. It takes several weeks after someone develops symptoms to get sick enough to be hospitalized and die. As more young people get infected, the greater the risk they will pass the virus on to more vulnerable people who have a greater chance of dying. That includes the elderly and anyone, regardless of age, with underlying conditions like diabetes.
“There are more cases. There are more hospitalizations in some of those places, and soon you’ll be seeing more deaths,” Fauci said in an interview last month with CNBC’s Meg Tirrell that was aired by the Milken Institute. “Even though the deaths are coming down as a country, that doesn’t mean that you’re not going to start seeing them coming up now.”
Beyond the number of deaths, scientists are still researching the long-term health consequences of contracting the virus. Some research has indicated the potential to cause long-term respiratory harm and damage to other organs.
“It’s a false narrative to take comfort in a lower rate of death,” Fauci said Tuesday during a livestream interview with Democratic Sen. Doug Jones, D-Ala. “There’s so many other things that are very dangerous and bad about this virus. Don’t get yourself into false complacency.”
.