Part 2 0f 2
Heart failure
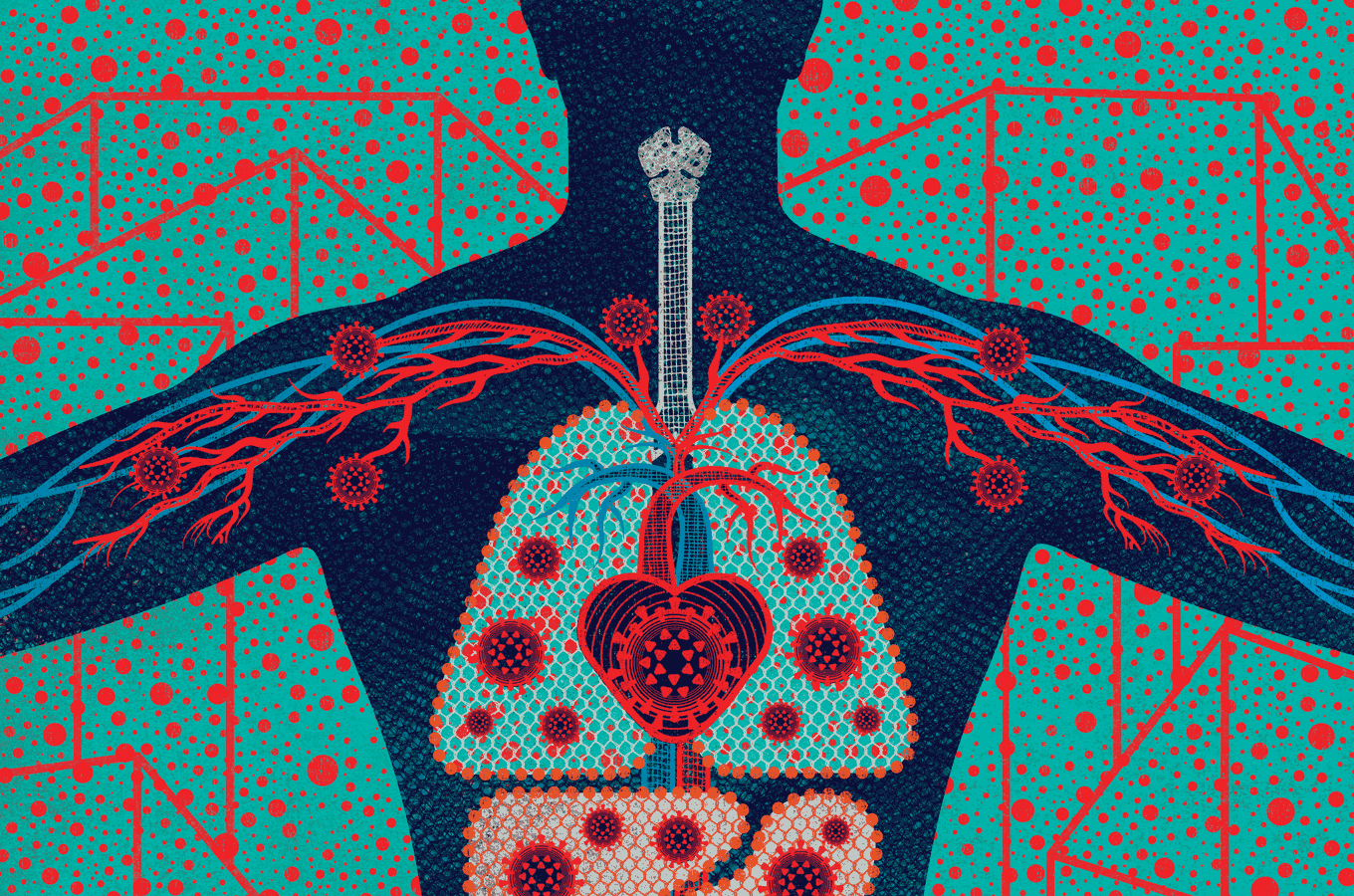
In April, Susan Parson, MD, a Bay Area medical examiner, made a startling discovery. For nearly two months, officials had believed that the first people in the U.S. to die from COVID-19 had died of respiratory failure in Washington state in late February. At the time, the U.S. Centers for Disease Control and Prevention limited testing to people who had respiratory symptoms and had recently traveled to China or otherwise been exposed to the virus. Those restrictions, however, turned out to be misguided.
As a medical examiner for California’s Santa Clara County, Parson had done a routine autopsy on a 57-year-old woman named Patricia Dowd, who had died suddenly at home on February 6. In Dowd’s tissues, Parson found the cause of her death: SARS-CoV-2. But the virus hadn’t wrecked Dowd’s lungs. In fact, she had only mild pneumonia. Instead, SARS-CoV-2 had ruptured her heart.
Meanwhile, epidemiologists began learning that preexisting heart disease and related conditions put people at greater risk of suffering and dying from COVID-19. “We’re finding that many patients who have more severe forms of the illness are obese, they are diabetic, they are hypertensive,” says cardiologist
Nisha Parikh, MD, a UCSF associate professor who specializes in population health research. Such risk factors, she says, are unusual. “They’re not ones that really stood out in prior epidemics.”
Clinicians, too, were seeing surprising numbers of COVID-19 patients develop heart problems – muscle weakness, inflammation, arrhythmias, even heart attacks. “We’re not used to respiratory viruses having such dire consequences on the heart in such apparently high numbers,” says cardiologist
Gregory Marcus, MD, MAS ’08, UCSF’s Endowed Professor of Atrial Fibrillation Research. Many patients whose hearts acted up also had failing lungs. But others had no other symptoms or, like Dowd, only mild ones.
Since March, Marcus has co-led one of the largest community surveys to better understand the spread of SARS-CoV-2 and its myriad effects. The study, dubbed COVID-19 Citizen Science, has so far enrolled more than 27,000 people; anyone with a smartphone
can participate. Marcus plans to also start collecting data from wearable devices, including Fitbits and Zio patches, which wirelessly monitor heart rhythms. “There may be large numbers of people who are suffering from cardiovascular effects of COVID-19 in the absence of other symptoms,” Marcus says. “I’m worried we’re missing those cases.”
It stands to reason that SARS-CoV-2 affects the heart. After all, heart cells are flush with ACE2 receptors, the virus’s vital port of entry. And, indeed, laboratory experiments suggest that the virus can enter and replicate in cultured human heart cells, says
Bruce Conklin, MD, a professor of medicine and an expert in heart-disease genetics at UCSF and the Gladstone Institutes.
But Conklin doesn’t think SARS-CoV-2 necessarily kills heart cells outright. Rather, in the process of copying itself, the virus steals pieces of the genetic instructions that tell the heart cells how to do their job. “It’s hauling away and hijacking stuff that’s necessary for the heart to beat,” he says. He is currently testing this hypothesis using human heart cells grown in cup-sized vessels in the lab of
Todd McDevitt, PhD, a bioengineer at UCSF and the Gladstone Institutes.
It’s also possible, however, that an infected person’s own immune system may do the majority of the damage in the heart, as it appears to do in the lungs. “The heart probably gets infected by a lot of other viruses, and they don’t have a lethal effect,” Conklin says. “What makes this one different?”
Graph with three bars. Bar at left has 80% at top and Non-Severe at bottom. Bar in middle has 15% at top and Severe at bottom Bar at right has 5% at top and Critical at bottom. Text below graph reads: Most symptomatic cases of COVID-19 are mild. To left of graph, small circle with the letter “i” in the middle opens to text reading: Graph Data: Wu et al., JAMA 2020. Livingston et al., JAMA 2020. Garg et al, MMWR 2020. Stoke et al., MMWR 2020. Left of graph: illustration of a coronavirus.
Most symptomatic cases of COVID-19 are mild.
Stranger things
Toward the end of March, as San Francisco began to warm up, Sonia got cold feet. She put on wool socks and turned up her heater. Still, her feet felt frozen. Three days later, her soles turned splotchy purple. Red dots appeared on her toes. At night, her cold feet itched and burned. Walking hurt. And she was exhausted, napping through afternoon Zoom meetings. “It was so bizarre,” says Sonia, a San Francisco resident. A week later, her symptoms were gone.
“Yes, COVID,” wrote
Lindy Fox, MD, a UCSF professor of dermatology, replying to an email describing Sonia’s case. Sonia wasn’t surprised. Anyone, like her, who’s been following news of the pandemic has probably heard about “COVID toes,” a painful or itchy skin rash that sometimes pops up in young adults with otherwise mild or asymptomatic cases of COVID-19.
“It looks like what we call pernio, or chilblains,” Fox says, “which is a pretty common phenomenon when somebody goes out in cold weather – they start to get purple or pink bumps on their fingers or toes.”
Many people with rashes like Sonia’s don’t test positive for COVID-19, Fox says, which has made some clinicians skeptical of the connection; when patients have both, it’s just a coincidence, they believe. But Fox doesn’t think so. For one thing, “the time of year is wrong,” she says. “Pernio usually shows up in the dead of winter.” Even more compelling, dermatologists around the world are “getting crazy numbers of calls about it,” Fox says. “In the last three weeks, I’ve had somewhere between 10 and 12 patients.
Normally, I have four a year.”
20%-40% of people with COVID-19 experience diarrhea, nausea, or vomiting before other symptoms.
And it’s not just dermatologists who are adding their observations to COVID-19’s ever-expanding symptom list. Gut specialists are finding that 20% to 40% of people with the disease experience diarrhea, nausea, or vomiting before other symptoms, says gastroenterologist
Michael Kattah, MD, PhD, a UCSF assistant professor. If you swallow virus particles, he says, there’s a good chance they will infect cells lining your stomach, small intestine, or colon. As in the lungs and heart, these cells are studded with vulnerable ACE2 portals.
Especially disconcerting, Kattah says, is how long the virus seems to persist in the gut. About 50% of patients with COVID-19 have virus particles in their stools, often for weeks after their nose swabs test negative, he points out. Laboratory studies show that these particles are often still alive and can infect cells in a petri dish. Whether fecal transmission occurs between people, however, is an open question. If the answer is yes, people recovering from COVID-19 may need to stay quarantined even after they feel well, and the rest of us will need to be as meticulous about bathroom hygiene as we’ve become about handwashing and mask-wearing.
Other specialists are also raising flags. Neurologists worry about reports of COVID-19 patients with headaches, “brain fog,” loss of the sense of smell, dizziness, delirium, and, in rare cases, stroke. Nephrologists worry about kidney stress and failure. Hepatologists worry about liver injuries. Ophthalmologists worry about pink eye. Pediatricians, meanwhile, worry about a peculiar
COVID-related inflammatory syndrome that’s showing up in kids and young adults.
There’s a lot of smoke. We need to figure out where the fire is coming from.”
MICHAEL WILSON, MD
Researchers are still sorting out the causes for this constellation of effects. If you come down with a particular symptom, is it because the virus is attacking your cells? Because your immune system is overreacting? Or just because you’re very sick? In any severe illness, for example, the kidneys must work extra hard to filter waste and control nutrients and fluid; if overtaxed, they may begin to fail. Similarly, cognitive problems can result from increased blood toxins due to stressed kidneys or from low oxygen due to respiratory distress. “There’s a lot of smoke,” says
Michael Wilson, MD ’07, MAS ’16, the Rachleff Distinguished Professor at UCSF’s Weill Institute for Neurosciences. “We need to figure out where the fire is coming from.”
Recently, there’s been speculation that some of COVID-19’s seemingly disparate symptoms may stem from trouble in the blood. Blood clots, for example, are showing up in cases of COVID-19 frequently enough for clinicians to take notice. “There’s something unique about the coagulation system in these patients,” says nephrologist
Kathleen Liu, MD ’99, PhD ’97, MAS ’07, a UCSF professor of medicine. In caring for COVID-19 patients on dialysis machines, she’s been surprised to see blood clots block dialysis tubes more than usual. Clotted tubes are common, she says, “but this is extreme.”
Evidence suggests SARS-CoV-2 can infect cells in the walls of blood vessels that help regulate clotting.
That may be because, as growing evidence suggests, SARS-CoV-2 can infect cells in the walls of blood vessels that help regulate blood flow and coagulation, or clotting. If true, this behavior could explain some of the virus’s weirder (and rarer) manifestations, such as heart attacks, strokes, and even “COVID toes.”
“Our vasculature is a contiguous system,” says cardiologist Parikh. “Thus injury in one area, such as blood vessels in the lungs, can set off clotting cascades that affect multiple organs.” Some of that trouble likely results from inflammation triggered by the immune system, she points out, although another culprit may be the body’s RAAS, or renin-angiotensin-aldosterone system, a hormone system that controls blood pressure and fluid balance. Because RAAS involves ACE2 receptors, Parikh suspects it may become disrupted when the virus infects cells through these receptors, thus triggering coagulation and other downstream effects. Her lab is now studying this system in COVID-19 patients to better understand how SARS-CoV-2 infection affects it.
Inevitably, some ailments may turn out to be red herrings. During a pandemic, when people are flocking to hospitals with infections, clinicians will also see a rise in other health problems, simply by the rules of statistics, points out
S. Andrew Josephson, MD, the Francheschi-Mitchell Professor, chair of UCSF’s neurology department, and a member of the Weill Institute for Neurosciences. “If the prevalence of infection is high, then almost any condition – a broken leg, if you will – you might conclude is associated with COVID-19.”
“As clinicians, we want to get information to our medical community and to the public as quickly as possible,” Josephson says, “but we have to be cautious about not making too big a deal of a little blip.”
The long tail
As with any infection, how long a bout of COVID-19 lasts
varies from person to person. If you’re ill enough to need critical care, you can expect the disease to take at least a few weeks to run its course. In some cases, symptoms persist for months. For a typical milder case, though, you should feel better within a couple weeks.
At that point, the question foremost on your mind will be: Am I immune? There are now more than a dozen antibody tests on the market, but most are unreliable,
according to UCSF research. And even the best tests can’t tell you whether you have enough of the right kinds of antibodies to protect you against reinfection. “There is a lot of hope and belief that we’ll have an antibody test that actually informs us of immunity, but we’re not quite there yet,” says
Chaz Langelier, MD, PhD, a UCSF assistant professor of medicine who is working to improve diagnostic tools for COVID-19.
What we have in the meantime are a lot of unknowns: If you do become immune to SARS-CoV-2, when and how does that occur? Will you gain immunity from a mild or asymptomatic case, as well as a severe one? How long will that immunity last?
“The answers will have huge implications for social distancing and masking and for getting the economy back up and running,” says
Michael Peluso, MD, a clinical fellow who came to UCSF three years ago to help fight HIV. Now he’s co-leading
a new study called LIINC (Long-term Impact of Infection with Novel Coronavirus), which is enrolling people who have been infected with SARS-CoV-2 and will follow them for two years. Besides illuminating changes in immunity over time, LIINC is investigating chronic effects of infection on the immune system, lungs, heart, brain, blood, and other parts of the body.
“I hope people will recover and immunity will be protective and long-lasting, and that will be that,” Peluso says.
It’s what we all hope. We hope we will beat an infection swiftly – or, better yet, avoid the virus until there is a vaccine. We hope that if we do fall gravely ill, we will be cared for by the best providers and tended to by people we love. The reality, as we already know, is more complicated. And even if COVID-19 doesn’t batter our bodies, the pandemic will surely leave scars – on our psyches, our livelihoods, our institutions, and our health – that we are only beginning to fathom. In truth, we don’t know how our cards will fall, as individuals or as a people. Only time – and data – will tell.















:watermark(cdn.texastribune.org/media/watermarks/2020.png,-0,30,0)/static.texastribune.org/media/files/a1410a41a992f0019007e2864fc9f9e6/DHR%20COVID%20Ward%20Edinburg%20MG%20TT%2029)