Since the summer of 2019, I've been speaking with one of the world's leading pandemic experts about what a global outbreak could look like. Now, as the world enters a grim new phase, he says we're in a whole new ball game.

www.cnet.com
(fair use applies)
'We'll be living with masks for years': COVID-19 through the eyes of a pandemic expert
Since the summer of 2019, I've been speaking with one of the world's leading pandemic experts about what a global outbreak could look like. Now, as the world enters a grim new phase, he says we're in a whole new ball game.
Claire Reilly
July 6, 2020 11:35 a.m. PT
Eric Toner has been planning for a pandemic for years. He's briefed world leaders on outbreaks and how to best prepare entire nations for mass casualties. He's simulated epidemics in real time and studied the world's response to major global health emergencies like SARS and the 1918 influenza pandemic.
But nothing could've prepared him for how the COVID-19 pandemic would play out.
Toner is a senior scholar at the Johns Hopkins Center for Health Security and a world leader in pandemic preparedness. The threat of a novel coronavirus is not new to him. In fact, in October 2019, Toner and the team at Johns Hopkins ran a coronavirus pandemic simulation in New York, months before COVID-19 started spreading across the world. As part of the half-day, tabletop exercise, Toner met with other health professionals to walk through a theoretical coronavirus outbreak and examine how governments and private businesses would respond.
Johns Hopkins has run these simulations for years, with Hollywood-sounding code names like Dark Winter (smallpox) and Clade X ("a biologically-engineered, intentionally-released airborne pathogen" which caused hundreds of millions of hypothetical deaths). The goal of the simulations is to help public health experts and policymakers better prepare for the eventual day a real pandemic arrives.
Now that day has come.
But simulating a pandemic is a far cry from watching the world handle an actual pandemic unfolding in real time. On that front, Toner says some countries are failing the test.
"The US response has been extraordinarily disappointing and wrongheaded," he told me via Zoom, at the end of June. "Whenever there's been an opportunity to do the right thing, we seem to have done the wrong thing. The US has to recognize that it is competing for first or second position of the worst affected country in the world."
Caught off guard
It's not the first time I've spoken to Toner about pandemics.
We first met in July 2019, when I traveled to the Johns Hopkins Center for Health Security in Baltimore to interview him about how the world would prepare for a pandemic. The interview was for "Hacking the Apocalypse" -- CNET's new documentary series looking at the tech solutions that could save us from doomsday events. Naturally, a series about terrifying global disasters had to include an episode on pandemics, but for me (and the rest of the team working on the series), this all felt theoretical. A kind of thought experiment that might play out in your head while you watch Contagion on TV.
But then came 2020. The world started to enter lockdown and words like "pandemic," "social distancing" and "quarantine" began embedding themselves in the daily vernacular. Our entire documentary series needed to be rewritten and recut. Suddenly, none of this was theoretical. And as I rewatched my original interview with Toner (conducted in a small room! Without face masks!) I kept rewinding the same part to play over and over.
"Is there a chance that we could be caught off guard by some sort of horrible, mutant bat influenza?" I had asked him on that day, five months before cases of the novel coronavirus were first reported.
"Yes," Toner replied. "And we probably will be."
I've spoken to Toner a number of times since then. Back in April, his assessment was grim.
"I think one would have to be clueless not to be scared right now," he told me, over a Zoom call from his home office. "The current coronavirus pandemic is worse than many that we have anticipated in the past ... this is going to end up being a truly historically bad event."
Now, as the world enters the second half of an entire year dominated by the pandemic, the situation is still just as serious.
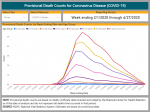
According to a July 1 update from Johns Hopkins (which has been tracking pandemic stats and providing regular situation reports), the pandemic has hit nearly every country across the world, with more than 10 million reported cases and more than half a million deaths. Of the more than 200 countries and territories reporting cases, 86 are reporting community transmission -- essentially, outbreaks that can't be traced to recent travel, other known cases or known clusters of the disease.
When I speak to Toner at the end of June, our mood has shifted. This is no longer an emerging threat. And unlike our previous conversations, I'm not expecting him to tell me about the quick fix that will end this crisis.
It's clear we're no longer in a sprint. We're in for a marathon.
'There will be no lull'
Many countries have seen success in the fight against the coronavirus, locking down early, moving quickly to adopt the World Health Organization's advice and ramping up diagnostic testing to identify and isolate localized outbreaks as they surfaced.
But as the northern hemisphere entered summer, hopes of flattening the curve in the US soon ran up against reports of cases continuing to rise as states reopened. Toner, though, is quick to talk down any mention of a "second wave."
"When you're underwater, it's really hard to tell how many waves are passing over you," Toner says. "I don't know whether it's a first wave or a second wave. I don't think it makes any difference. There is a resurgence of cases that, in some states, looks like just a continuation of their outbreaks. In other states, it'll look more like a second wave.
"I think what's important is that there's going to be no summertime lull with a big wave in the fall. It's clear that we are having a significant resurgence of cases in the summer, and they'll get bigger. And it'll keep going until we lock things down again."
Unlike the influenza virus, which was behind the 1918 pandemic that claimed as many as 50 million to 100 million lives around the world, Toner says there's no good evidence of seasonality with COVID-19. Until we have a vaccine, any rise or fall in cases will be based on social factors: communities locking down and families sheltering in place. And, as was the case back in 1918, individuals wearing masks.
There is some good news to come out of the first six months of the pandemic. Hospitals are getting better at managing symptoms and intervening before cases reach a point of no return, helping to reduce the death rate. He points to therapies like remdesivir, which has shown positive effects in trials and has been authorized for hospitalized COVID patients, and convalescent plasma therapy, which could be used as a way to transfer a level of immunity to sick patients.
But there's no silver bullet. Experts agree that it will be at least a year from now before we have a vaccine that's accessible to most people. Mass immunization likely won't come until 2022, and even then, Toner says vaccination may require a double dose to be effective.
And until then?
"I think that mask wearing and some degree of social distancing, we will be living with -- hopefully living with happily -- for several years," he says.
For many of us, this long timeline can lead to a feeling of hopelessness. But Toner says there's a way to control our future, and it's not all that different from the advice he's given in simulations, advice that dates back more than a century.
"It's actually pretty straightforward. If we cover our faces, and both you and anyone you're interacting with are wearing a mask, the risk of transmission goes way down. Being outside, having distance between you and other people reduces the risk of transmission dramatically.
"There are a lot of things you can do and maintain those conditions. If you spread out, if you maintain distance, if you avoid crowded places, you could go to a beach, you go to the mountains, you could go to a lake, you can do things outside without a problem."
As for those who refuse to wear a mask, Toner doesn't mince his words.
"They will get over it," he says. "It's just a question of how many people get sick and die before they get over it."
.




















 The Louvre museum reopens its doors after 16-week closure as...
The Louvre museum reopens its doors after 16-week closure as... Holidaymakers face frustrating wait hoping for their money...
Holidaymakers face frustrating wait hoping for their money...