[COMMENT: I had read that this E.O. had more in it than the MSM covered. So I thought I would post it.]
In December 2019, a novel coronavirus known as SARS-CoV-2 ("the virus") was first detected in Wuhan, Hubei Province, People's Republic of China, causing an

www.whitehouse.gov
Executive Order on Regulatory Relief to Support Economic Recovery
ECONOMY & JOBS
Issued on: May 19, 2020
 ALL NEWS
ALL NEWS
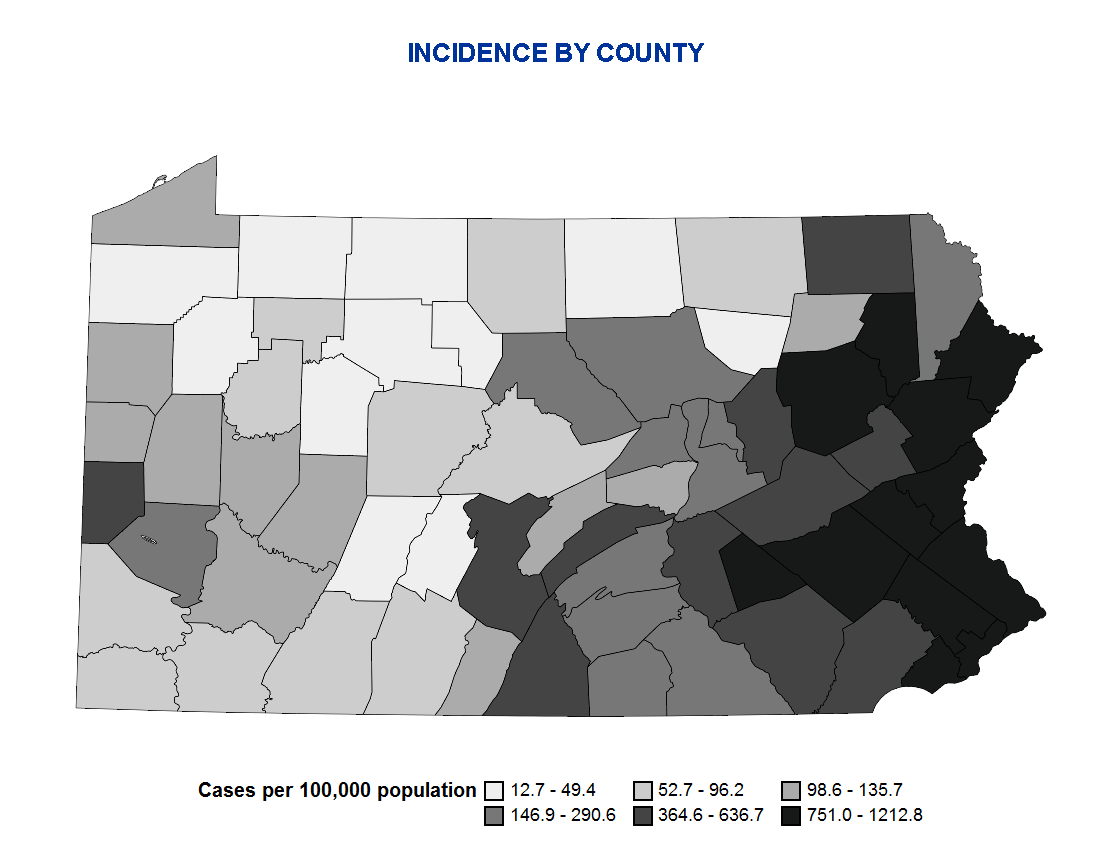
In December 2019, a novel coronavirus known as SARS-CoV-2 (“the virus”) was first detected in Wuhan, Hubei Province, People’s Republic of China, causing an outbreak of the disease COVID-19, which has now spread globally. The Secretary of Health and Human Services declared a public health emergency on January 31, 2020, under section 319 of the Public Health Service Act (42 U.S.C. 247d), in response to COVID-19. In Proclamation 9994 of March 13, 2020 (Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak), I declared that the COVID-19 outbreak in the United States constituted a national emergency, beginning March 1, 2020.
I have taken sweeping action to control the spread of the virus in the United States, including by suspending entry of certain foreign nationals who present a risk of transmitting the virus; implementing policies to accelerate acquisition of personal protective equipment and bring new diagnostic capabilities to laboratories; and pressing forward rapidly in the search for effective treatments and vaccines. Our States, tribes, territories, local communities, health authorities, hospitals, doctors and nurses, manufacturers, and critical infrastructure workers have all performed heroic service on the front lines battling COVID-19. Executive departments and agencies (agencies), under my leadership, have helped them by taking hundreds of administrative actions since March, many of which provided flexibility regarding burdensome requirements that stood in the way of implementing the most effective strategies to stop the virus’s spread.
The virus has attacked our Nation’s economy as well as its health. Many businesses and non-profits have been forced to close or lay off workers, and in the last 8 weeks, the Nation has seen more than 36 million new unemployment insurance claims. I have worked with the Congress to provide vital relief to small businesses to keep workers employed and to bring assistance to those who have lost their jobs. On April 16, 2020, I announced Guidelines for Opening Up America Again, a framework for safely re-opening the country and putting millions of Americans back to work.
Just as we continue to battle COVID-19 itself, so too must we now join together to overcome the effects the virus has had on our economy. Success will require the efforts not only of the Federal Government, but also of every State, tribe, territory, and locality; of businesses, non-profits, and houses of worship; and of the American people. To aid those efforts,
agencies must continue to remove barriers to the greatest engine of economic prosperity the world has ever known: the innovation, initiative, and drive of the American people.
By the authority vested in me as President by the Constitution and the laws of the United States of America, it is hereby ordered as follows:
Section 1.
Policy. It is the policy of the United States to combat the economic consequences of COVID-19 with the same vigor and resourcefulness with which the fight against COVID-19 itself has been waged.
Agencies should address this economic emergency by rescinding, modifying, waiving, or providing exemptions from regulations and other requirements that may inhibit economic recovery, consistent with applicable law and with protection of the public health and safety, with national and homeland security, and with budgetary priorities and operational feasibility. They should also give businesses, especially small businesses, the confidence they need to re-open by providing guidance on what the law requires; by recognizing the efforts of businesses to comply with often-complex regulations in complicated and swiftly changing circumstances; and by committing to fairness in administrative enforcement and adjudication.
Sec.
2.
Definitions. (a) “Emergency authorities” means any statutory or regulatory authorities or exceptions that authorize action in an emergency, in exigent circumstances, for good cause, or in similar situations.
(b) “Agency” has the meaning given in section 3502 of title 44, United States Code.
(c) “Administrative enforcement” includes investigations, assertions of statutory or regulatory violations, and adjudications by adjudicators as defined herein.
(d) “Adjudicator” means an agency official who makes a determination that has legal consequence, as defined in section 2(d) of Executive Order 13892 of October 9, 2019 (Promoting the Rule of Law Through Transparency and Fairness in Civil Administrative Enforcement and Adjudication), for a person, except that it does not mean the head of an agency, a member of a multi-member board that heads an agency, or a Presidential appointee.
(e) “Pre-enforcement ruling” has the meaning given it in section 2(f) of Executive Order 13892.
(f) “Regulatory standard” includes any requirement imposed on the public by a Federal regulation, as defined in section 2(g) of Executive Order 13892, or any recommendation, best practice, standard, or other, similar provision of a Federal guidance document as defined in section 2(c) of Executive Order 13892.
(g) “Unfair surprise” has the meaning given it in section 2(e) of Executive Order 13892.
Sec.
3.
Federal Response.
The heads of all agencies are directed to use, to the fullest extent possible and consistent with applicable law, any emergency authorities that I have previously invoked in response to the COVID-19 outbreak or that are otherwise available to them to support the economic response to the COVID-19 outbreak. The heads of all agencies are also encouraged to promote economic recovery through non-regulatory actions.
Sec.
4.
Rescission and waiver of regulatory standards.
The heads of all agencies shall identify regulatory standards that may inhibit economic recovery and shall consider taking appropriate action, consistent with applicable law, including by issuing proposed rules as necessary, to temporarily or permanently rescind, modify, waive, or exempt persons or entities from those requirements, and to consider exercising appropriate temporary enforcement discretion or appropriate temporary extensions of time as provided for in enforceable agreements with respect to those requirements, for the purpose of promoting job creation and economic growth, insofar as doing so is consistent with the law and with the policy considerations identified in section 1 of this order.
Sec.
5.
Compliance assistance for regulated entities. (a) The heads of all agencies, excluding the Department of Justice, shall accelerate procedures by which a regulated person or entity may receive a pre-enforcement ruling under Executive Order 13892 with respect to whether proposed conduct in response to the COVID-19 outbreak, including any response to legislative or executive economic stimulus actions, is consistent with statutes and regulations administered by the agency, insofar as doing so is consistent with the law and with the policy considerations identified in section 1 of this order.
Pre‑enforcement rulings under this subsection may be issued without regard to the requirements of section 6(a) of Executive Order 13892.
(b) The heads of all agencies shall consider whether to formulate, and make public, policies of enforcement discretion that, as permitted by law and as appropriate in the context of particular statutory and regulatory programs and the policy considerations identified in section 1 of this order, decline enforcement against persons and entities that have attempted in reasonable good faith to comply with applicable statutory and regulatory standards, including those persons and entities acting in conformity with a pre-enforcement ruling.
(c) As a result of the ongoing COVID-19 pandemic, the Department of Health and Human Services, including through the Centers for Disease Control and Prevention, and other agencies have issued, or plan to issue in the future, guidance on action suggested to stem the transmission and spread of that disease. In formulating any policies of enforcement discretion undersubsection (b) of this section, an agency head should consider a situation in which a person or entity makes a reasonable attempt to comply with such guidance, which the person or entity reasonably deems applicable to its circumstances, to be a rationale for declining enforcement under subsection (b) of this section.
Non-adherence to guidance shall not by itself form the basis for an enforcement action by a Federal agency.
Sec.
6.
Fairness in Administrative Enforcement and Adjudication. The heads of all agencies shall consider the principles of fairness in administrative enforcement and adjudication listed below, and revise their procedures and practices in light of them, consistent with applicable law and as they deem appropriate in the context of particular statutory and regulatory programs and the policy considerations identified in section 1 of this order.
(a) The Government should bear the burden of proving an alleged violation of law; the subject of enforcement should not bear the burden of proving compliance.
(b) Administrative enforcement should be prompt and fair.
(c) Administrative adjudicators should be independent of enforcement staff.
(d) Consistent with any executive branch confidentiality interests, the Government should provide favorable relevant evidence in possession of the agency to the subject of an administrative enforcement action.
(e) All rules of evidence and procedure should be public, clear, and effective.
(f) Penalties should be proportionate, transparent, and imposed in adherence to consistent standards and only as authorized by law.
(g) Administrative enforcement should be free of improper Government coercion.
(h) Liability should be imposed only for violations of statutes or duly issued regulations, after notice and an opportunity to respond.
(i) Administrative enforcement should be free of unfair surprise.
(j) Agencies must be accountable for their administrative enforcement decisions.
Sec.
7.
Review of Regulatory Response.
The heads of all agencies shall review any regulatory standards they have temporarily rescinded, suspended, modified, or waived during the public health emergency, any such actions they take pursuant to section 4 of this order, and other regulatory flexibilities they have implemented in response to COVID-19, whether before or after issuance of this order, and determine which, if any, would promote economic recovery if made permanent, insofar as doing so is consistent with the policy considerations identified in section 1 of this order, and report the results of such review to the Director of the Office of Management and Budget, the Assistant to the President for Domestic Policy, and the Assistant to the President for Economic Policy.
Sec.
8.
Implementation. The Director of the Office of Management and Budget, in consultation with the Assistant to the President for Domestic Policy and the Assistant to the President for Economic Policy, shall monitor compliance with this order and may also issue memoranda providing guidance for implementing this order, including by setting deadlines for the reviews and reports required under section 7 of this order.
Sec.
9. General Provisions. (a) Nothing in this order shall be construed to impair or otherwise affect:
(i) the authority granted by law to an executive department or agency, or the head thereof; or
(ii) the functions of the Director of the Office of Management and Budget relating to budgetary, administrative, or legislative proposals.
(b) This order shall be implemented consistent with applicable law and subject to the availability of appropriations.
(c) Notwithstanding any other provision in this order, nothing in this order shall apply to any action that pertains to foreign or military affairs, or to a national security or homeland security function of the United States (other than procurement actions and actions involving the import or export of non-defense articles and services).
(d) This order is not intended to, and does not, create any right or benefit, substantive or procedural, enforceable at law or in equity by any party against the United States, its departments, agencies, or entities, its officers, employees, or agents, or any other person.

The White House



 ALL NEWS
ALL NEWS