Part 3 of 3
The dark side of ventilators: Those hooked up for long periods face difficult recoveries
Although the machines can mean the difference between life or death, they often cause other complications.
Medical staff, wearing protective suits and face masks, work at the intensive care unit for coronavirus disease patients at Ambroise Pare clinic in Neuilly-sur-Seine, near Paris. (Benoit Tessier/Reuters)
By
Carolyn Y. Johnson and
Ariana Eunjung Cha
April 6, 2020 at 10:25 a.m. PDT
For people desperately ill with covid-19, getting hooked up to a mechanical ventilator can mean the difference between life and death. But despite officials’ frantic efforts to secure more of the machines, they are not a magic bullet.
Many attached to the scarce machines will not make it out of the hospital. Data from
China, Italy and the
U.S. suggest that about half of those with covid-19 who receive ventilator support will die.
“They’re called life support for a reason — they just keep people alive while typically buying time for something else to heal the lungs,” said Scott Halpern, a bioethicist at the University of Pennsylvania. But with covid-19, the disease caused by the novel
coronavirus, “we don’t have a treatment for the underlying insult.”
For those who manage to defeat the virus and come off ventilators, the really hard part begins. Many will suffer long-term physical, mental and emotional issues, according to a staggering body of medical and scientific studies. Even a year after leaving the intensive care unit, many people experience
post-traumatic stress disorder,
Alzheimer’s-like cognitive deficits, depression,
lost jobs and problems with daily activities such as bathing and eating.
AD
“I think what we’re going to see is a wave, about six weeks after the initial illness,” said Samuel Brown, director of the Center for Humanizing Critical Care at Intermountain Healthcare in Utah. “One to three weeks to get off the ventilator, and a couple of weeks to get their sea legs back to get home — and then to finally realize: What happened? What did I just survive? And how desperately frightening that experience was for a wave of survivors who are going to have really difficult psychological symptoms.”
Although the vast majority of people with covid-19 experience
mild cases of infection, about one in six known cases develop severe shortness of breath. About half of those become critically ill, as people’s damaged lungs fill with fluid, staying alive only with the help of a mechanical ventilator, according to
evolving data.
By the end of the pandemic,
hundreds of thousands of Americans who have survived severe cases of covid-19 are likely to seed the next health-care crisis as many struggle with the physical and psychological effects of long hospital stays, say epidemiologists.
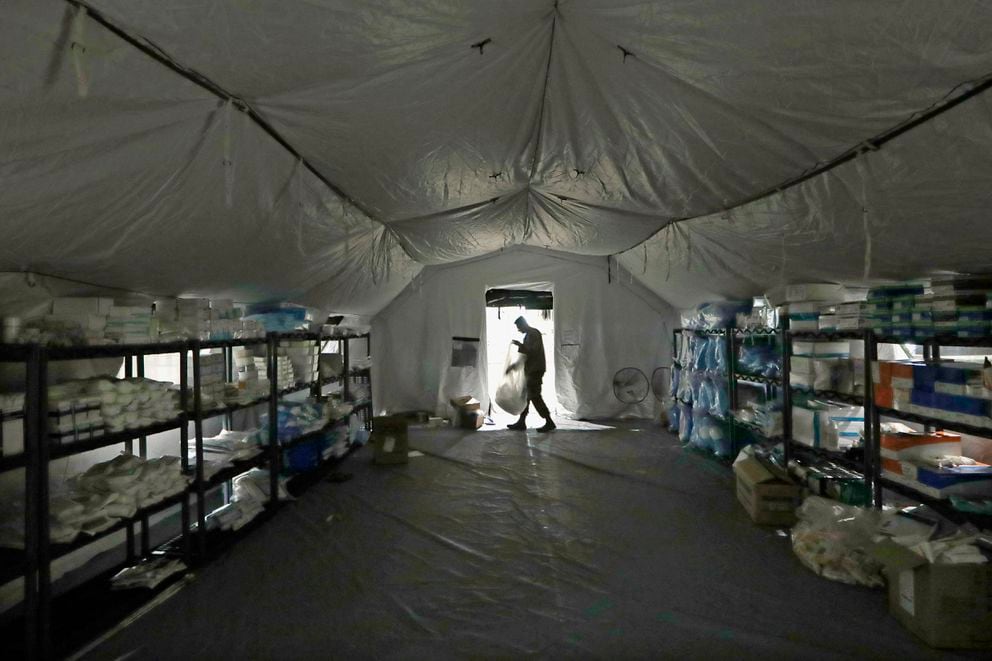
Patients with covid-19 typically stay on ventilators for prolonged periods which increases the likelihood of long-term complications. The risk of infection also means they are cut off from human contact, which also increases the risk of psychological issues.
“We normally kneel at their bedside and hold their hand and ask them, ‘How are you’ and tell them, ‘It is my privilege to help you.’ Instead what they are getting is someone in spacesuit garb with very little time to spend with them,” said E. Wesley Ely, a professor at Vanderbilt University in Nashville.
He recounted how a medical resident recently came to him in tears.
“I don’t feel like I’m a doctor,” the resident told Ely. “The first time I really sat with that patient was to pronounce him dead.”
Nic Brown scribbled this message to health-care workers at Cleveland Clinic who cared for him while he was hospitalized for covid-19: “I think you are all rock stars. … Today I leave this ICU a changed person, hopefully for the better." (Courtesy Cleveland Clinic)
ICU Survivors
The ranks of covid-19 survivors are just beginning to expand in the United States, but acute respiratory distress syndrome — the lung failure that kills patients — is also caused by other infections, giving doctors a deep reservoir of knowledge about what happens to such people after they leave the hospital.
Each year, there are about
200,000 people with acute respiratory distress in the United States, and about 60 percent of them live. Many of these survivors have been watching the unfolding pandemic in the United States with an unsettling sense of foresight and empathy.
A common complication of prolonged stays in intensive care units is something called “
ICU delirium,” in which patients become severely confused and may have nightmarish hallucinations — which could be worse if people never see their caregivers’ faces and don’t have family there to help them understand what really happened.
Nic Brown, a 38-year-old information technology manager, spent 18 days at the hospital — seven on a ventilator. He was Cleveland Clinic’s first covid-19 patient and said he has more memories of the ICU than he cares to remember.
“I had these horrible dreams and it was night after night of torment,” he said in an interview. “There was a point I wanted to ask them to pull the plug. I couldn’t do it.”
Brown was lucky. His condition improved after doctors treated him with a variety of experimental medications, and he was discharged last week. His lungs are still struggling to recover, and when he does ordinary things like stand up to check his computer printer, he gets winded. He also said he’s experienced some vision issues and, earlier on, confusion. He would write something down, but it wouldn’t match the message he intended to convey.
“When you typically get out of the ICU at the hospital, you get all this support like physical therapy and speech therapy but when you are a covid-19 patient, you get none of that,” he said.
With the risk of infection and social distancing orders in place, doctors say, many rehabilitation services have not been accepting patients recovering from the virus.
Michelle and Ken Bryden of Ellicott City, Md. A year ago, Michelle Bryden spent four days on a ventilator because of acute respiratory distress syndrome, which also occurs in covid-19. (Courtesy of Michelle Bryden)
Michelle Bryden, a 49-year-old engineer from Ellicott City, Md., was able to take advantage of that kind of support after her hospitalization for bacterial meningitis and sepsis left her on a ventilator for four days. She has been thinking about people recovering from covid-19 as she approaches the first anniversary of her hospitalization, imagining what her path through the medical system would have been like if she had been alone.
Bryden’s husband, Ken, was with her constantly in the hospital and has helped her fill in the gaps in her memory from when she was sedated and had no idea what was happening. But when he left the hospital to shower or sleep, the isolation was difficult, even though she knew he would soon return.
“Having him there was important, and I think not having visitors in the hospital would be so hard,” Bryden recalled. “I found the nights to be very scary.”
Eileen Rubin, now 57, who spent eight weeks on a ventilator due to acute respiratory distress syndrome caused by sepsis when she was 33, said that she isn’t sure she would have survived without her family’s presence and support.
“I cry for them [covid-19 patients], really, because they don’t have that support that is really so significant and meaningful, and there’s no way to change that,” Rubin said. “It’s a feeling you have that you carry with you. … You know somebody is fighting for you when you can’t fight for yourself.”
Health-care teams are finding ways to alleviate patients’ isolation, knowing that even small changes could mean the difference between a person who survives and one who is better-equipped to recover. Some health-care workers have put their photos in patients’ rooms so that when they come in covered in a mask and gown, they can point to the photo and say, “I’m that person.”
Others are communicating with telehealth apps from inside the hospital, so that they can at least have some face-to-face interactions, albeit on screen. Still others have used their private cellphones covered in zip-top bags to bring family members to the bedside with video chat. The Mayo Clinic recently brought up video chat on iPads to make sure that patients can see their families as they fight the virus alone.
Psychological risks
Even when people survive the illness, they will likely reenter a world where much of their support network simply can’t give them a hug due to social distancing guidelines — and where fear of contagion could create stigma, too.
“I think that’s a dynamic you can’t overemphasize — that it is always bad to be in the ICU, but it’s probably doubly bad to be in the ICU during a pandemic, because of the anxiety that is just fomenting,” said James Jackson, a psychologist at Vanderbilt University. “It’s in the air, if you will. And that all adds to the psychological burden.”
Just as combat veterans may not want to ever return to the battlefield, people who recover from critical illness may not even want to drive by the hospital, Jackson said — and that means that post-traumatic stress disorder could compound other medical problems, impeding people’s ability to seek the medical support they need.
How ventilators work and why we need them to fight covid-19
Coronavirus may cause a shortage of ventilators, and U.S. health-care workers are worried there won't be enough of them to serve covid-19 patients. (Daron Taylor/The Washington Post)
Centers to support ICU survivors are not at every hospital, and delivering additional care for a person’s physical, cognitive and mental health during a pandemic will be harder. Recovery may also be affected by the absence of family members in the hospital, as people trying to support their loved one may have little idea what they experienced.
“So now you have the family member who survived, and they’ve been through war. But no one really knows what that war experience was like,” said Michael Wilson, a pulmonary intensive care unit physician at Mayo Clinic.
It’s at home, after the first few weeks of convalescence, when people begin to try to bathe themselves or feed themselves that most people begin to grapple with limitations they may not have recognized in the hospital. They begin to reconstruct the lost time, piecing together fragments of memories. People may feel depressed as they realize that they have left the hospital — only to navigate a new set of problems that often last six months to a year.
“When someone is critically ill and so sick they require life support, such as a mechanical ventilator, most patients do not return to that former state when the life support is discontinued — particularly in the context of covid” where they may be on ventilators for long periods, said Dale Needham, professor of pulmonary and critical care medicine at Johns Hopkins University School of Medicine.
Bryden, for example, knows that she’s considered to be a “good” recovery case and is glad, because she’s not sure she could have handled worse. She lost 20 pounds of muscle. She had to learn how to get out of bed and use a walker, although she had once exercised every morning. She was cleared to eat food, but she tried eating rice, and the simple act of coordinating the movement of her mouth to chew and push food into her throat was impossible at first.
Bryden was able to return to work in six weeks, walking with a cane, and by six months, she says, she began to feel like herself.
“I would just emphasize that it is hard, and the fact you’ve gotten out of the ICU or the hospital is really only half the battle,” Bryden said, of the advice she would give people recovering from the worst cases of covid-19. “From the patient perspective, it was harder after I got out.”















:quality(70)/arc-anglerfish-arc2-prod-adn.s3.amazonaws.com/public/OE4UAGAIQZFWDILVKJA7IIDKVM.JPG)


















 I've noticed while watching the evening/nightly snooze, it appears to me that the media is rapidly portraying this pandemic in the US as a racial issue and more and more politicos are jumping on the bandwagon. I'm very confident that COVID isn't racist. The virus is statistically affecting folks that have other health probs like being overweight, diabetes, high blood pressure, etc. It just happens to be that alot of black / brown folk have those health issues and are getting sick with the virus. Its the same with white folk too. And Asians and pretty much everyone else. They are just comparing numbers and picking out the stuff they WANT to see and ignore all the other variables. The whole thing makes me
I've noticed while watching the evening/nightly snooze, it appears to me that the media is rapidly portraying this pandemic in the US as a racial issue and more and more politicos are jumping on the bandwagon. I'm very confident that COVID isn't racist. The virus is statistically affecting folks that have other health probs like being overweight, diabetes, high blood pressure, etc. It just happens to be that alot of black / brown folk have those health issues and are getting sick with the virus. Its the same with white folk too. And Asians and pretty much everyone else. They are just comparing numbers and picking out the stuff they WANT to see and ignore all the other variables. The whole thing makes me 


